Anatomy
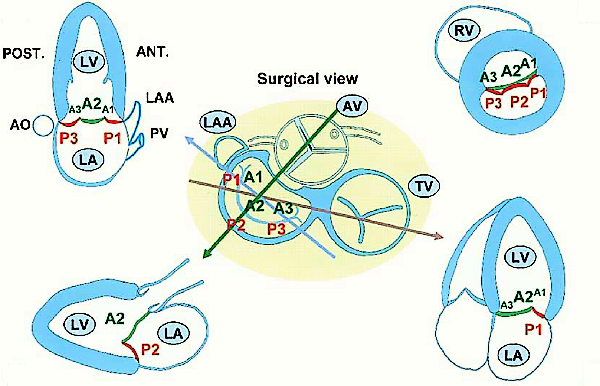
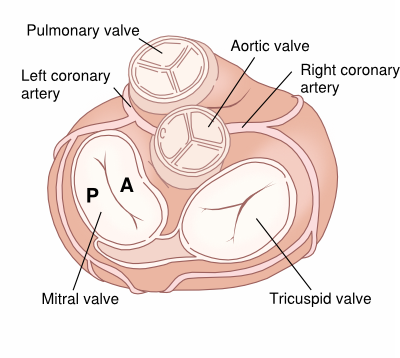
The mitral valve consists of two leaflets, the anterior (A) and the posterior valve leaflet (P), which together have a surface area of 4-6cm. At the inner edges of the leaflets chordae tendinae are attached, which ensure that the leaflets did not prolapse back into the atria during systole. The chordae attach to two large papillary muscles, that are part of the muscular tissue of the left ventricle.
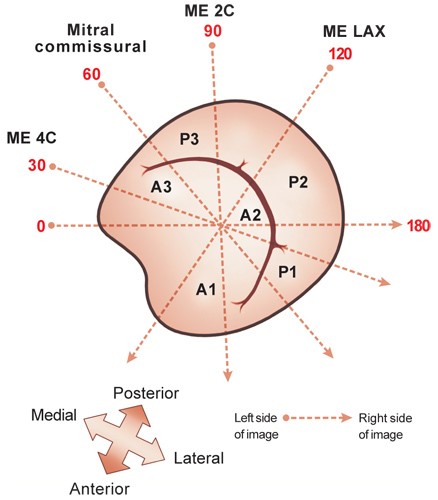
The mitral valve can be visualized in many views: PLAX, PSAXmv, AP4Ch, AP5Ch, AP2Ch, AP3Ch and subcostaal4Ch. A prolapse of the MV is best assessed on PLAX. However, mitral regurgitation should be assessed in all views. In case of major abnormalities of the mitral valve 3D TEE has additional value in assessing the anatomy and function.
Scallop partition of mitral valve