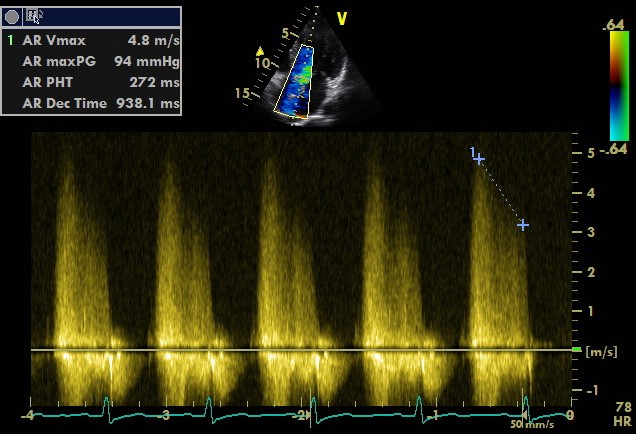
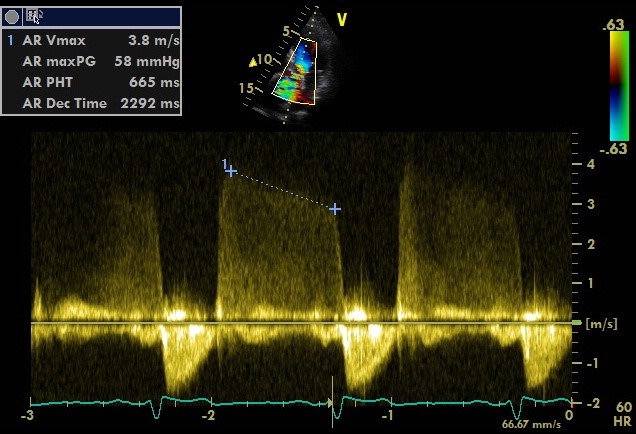
Bernoulli's principle
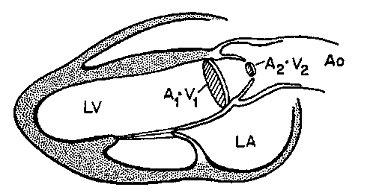
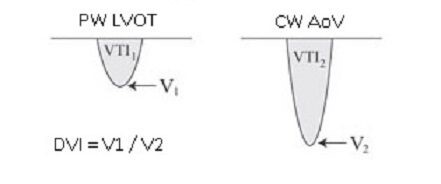
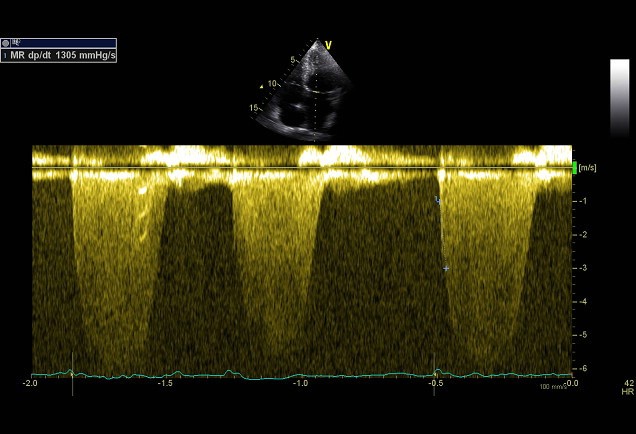
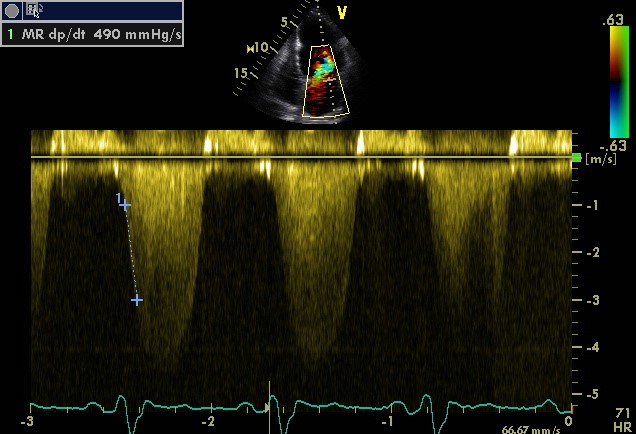
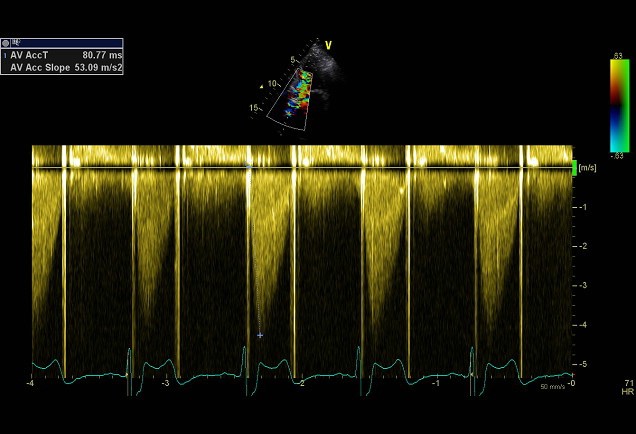
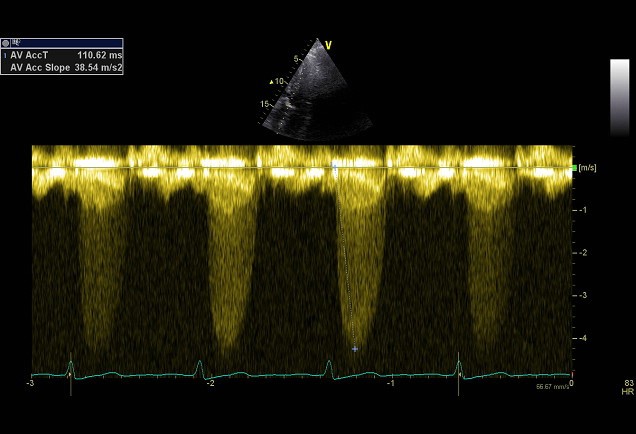
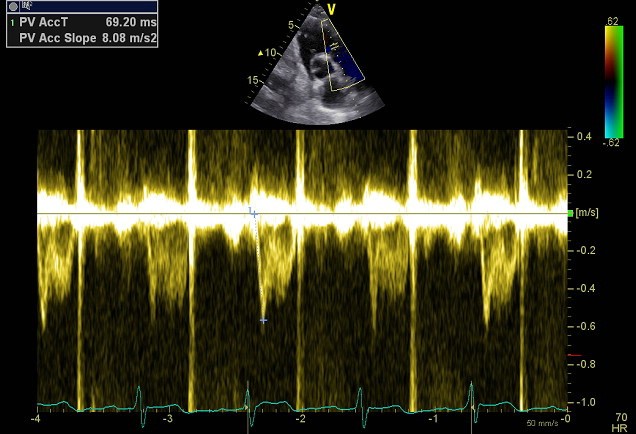
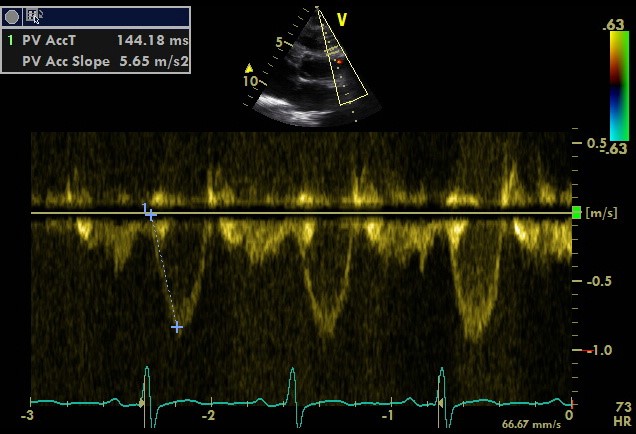
Simplified formula for converting velocity difference obtained by spectral Doppler to instantaneous pressure gradient. This clinical equation has been derived from the more complex Bernoulli equation by assuming that viscous losses and acceleration effects are negligible and by using an approximation for the constant that relates to the mass density of blood, a conversion factor for measurement units. In addition, the simplified Bernoulli equation assumes that the proximal velocity can be ignored, a reasonable assumption when velocity is <1 m/s because squaring a number <1 makes it even smaller. When the proximal velocity (V1) is over >1.5 m/s or the aortic velocity (V2) is >3.0 m/s, the proximal velocity should be included in the Bernoulli equation.
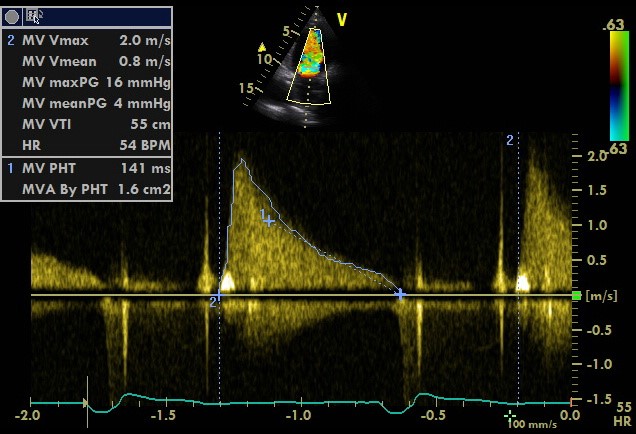
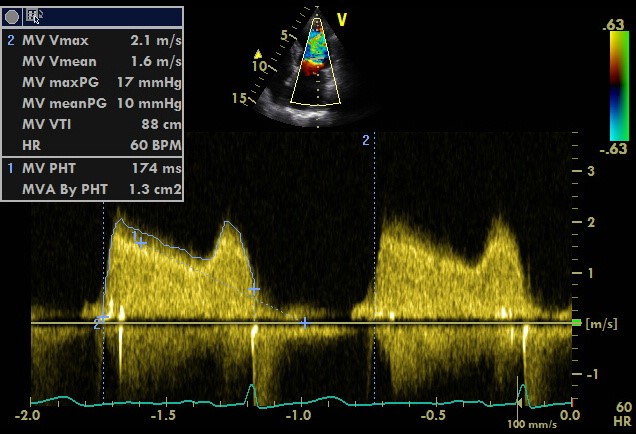
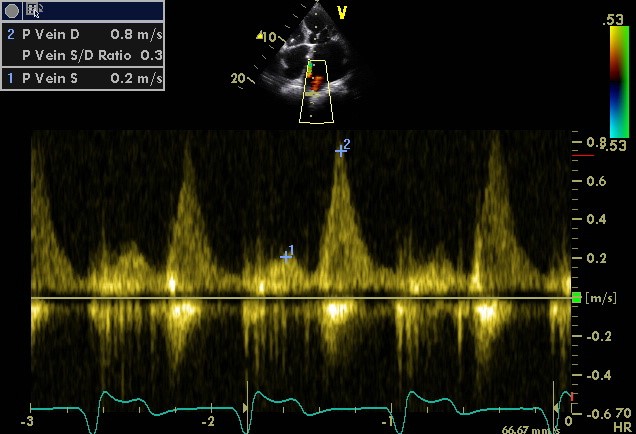
Calculation
ΔP = P2 − P1 = 4 • (V2² − V1²)
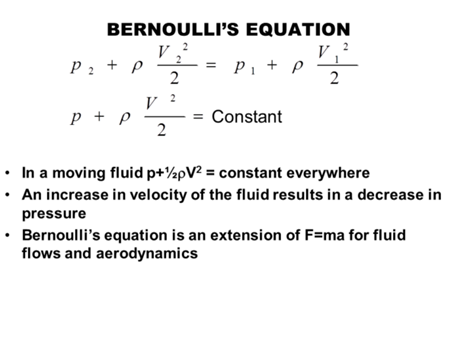
J Am Soc Echocardiogr. 2009 Jan;22(1):1-23