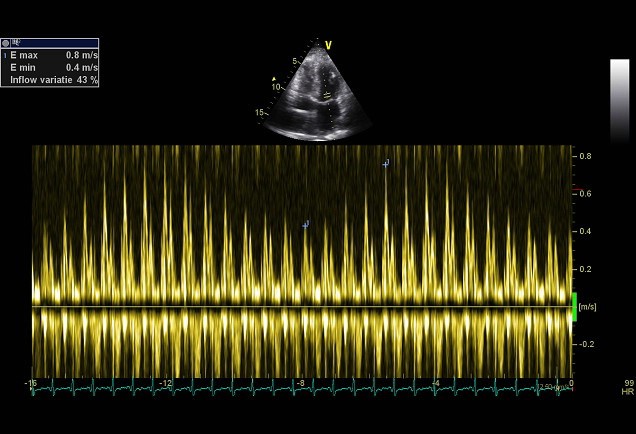
The RV early diastolic filling velocity is augmented with inspiration, while the LV diastolic filling velocity is diminished. The E/A ratio of the mitral and tricuspid-inflow pattern will be >1. The deceleration time of the mitral E-wave will also be shortened (>180 msec.) In the pulmonary vein flow, the S-wave will be smaller than the D-wave.?This is different in a constrictive pericarditis. A respiratory variation in MV inflow (at at the beginning of inspiration increase of the E-wave >25%) and TV inflow (at the beginning of inspiration increase of the E-wave >40%) is seen. Also a respiratory variation in the pulmonary vein is seen, in which the flow at the beginning of expiration, the diastolic forward flow increases >10%. This respiratory variation can also be observed at atrial fibrillation and in patients with severe obstructive lung disease. In these cases the flow from the vena cava towards the RV will increase However in a constrictive pericarditis, the flow will not increase. After a pericardectomy an abnormal filling pattern is often observed. It is believed that this is due to incomplete pericardectomy. On the other hand the myocardium sometimes is involved in the disease process. The early diastolic velocity of the septal mitral valve annulus (é) is often reduced postoperatively, which indicates a relaxation disorder of the myocardium. This could be explained by increased myocardial fibrosis found at autopsies. Development of constrictive pericarditis after pericardectomy is associated with a worse prognosis.
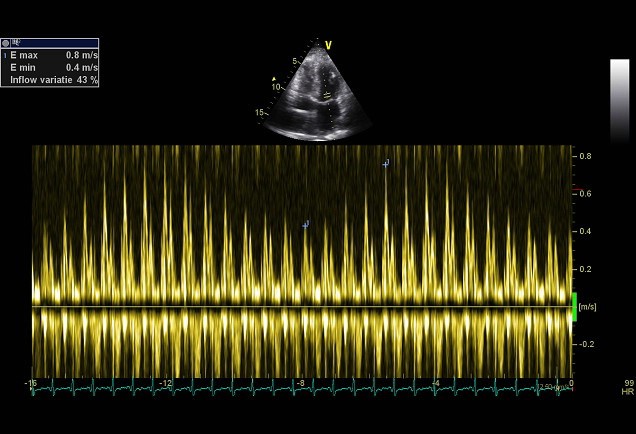
Respiratory flow variation >25%