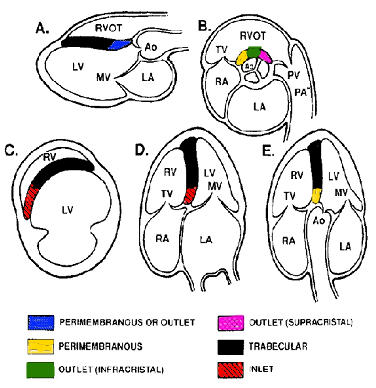
The ventricular septal defect (VSD) is a common congenital heart defect. Due to spontaneous closure during growth the VSD is less often seen in adulthood. VSD’s are divided into three groups: perimembranous, muscular and subarterial. The supracristal outlet VSD is called a subarterial VSD. A subarterial VSD can result in progressive aortic valve insufficiency, due to the lack of the cusp support by the outlet portion of the septum. In some cases even small subarterial VSD’s should be treated surgically. In some circumstances, the septal leaflet of the tricuspid valve can (partially) cover the perimembranous VSD. In these case the images can mimic a septal aneurysm.