Ischemia testing: DSE to detect ischemia
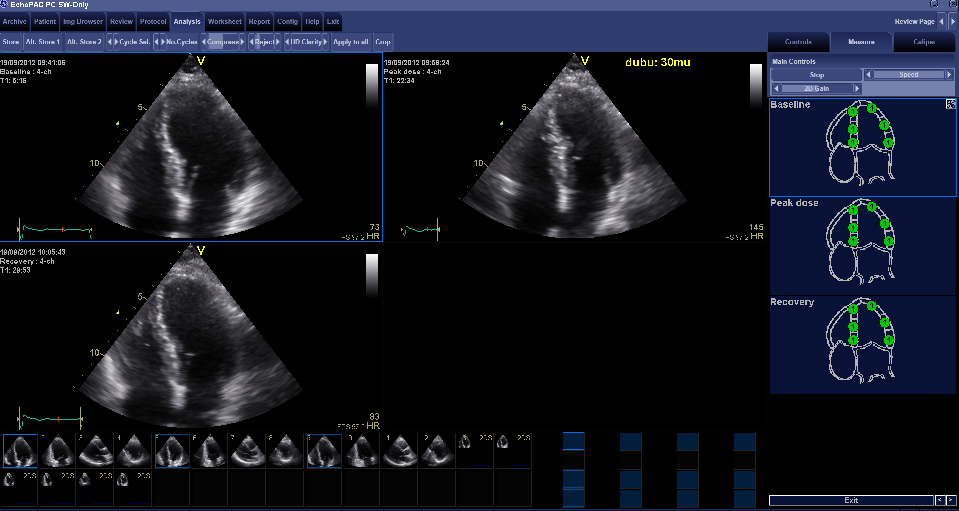
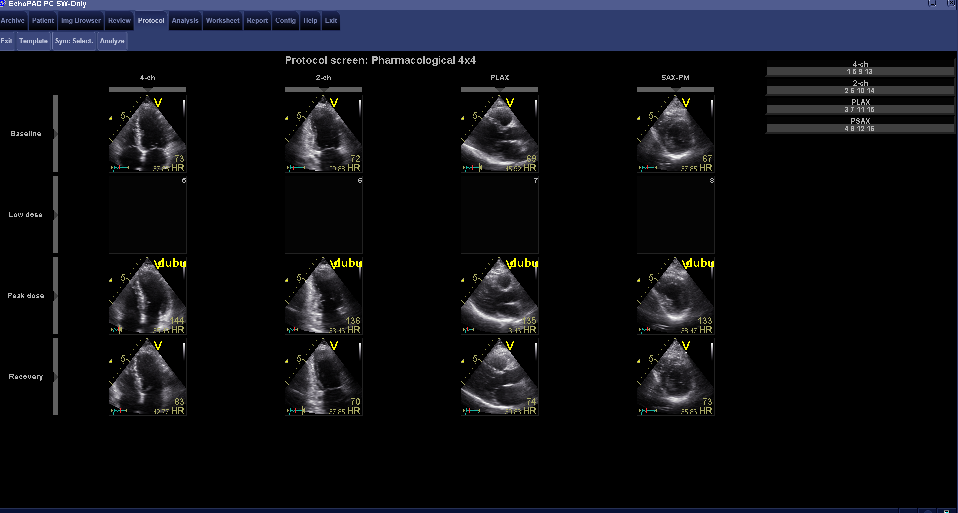
A stress echo is a study which evaluates the function of the LV in rest and during exercise. Ischemia can be provoked by stimulation of the heart by Dobutamine via a drip. Dobutamine is a catecholamine with predominant β-receptor stimulation, which causes positive inotropic, chronotropic and dromotropic effects on the heart. Dobutamine has a half-life of approximately 2 minutes. The inotropic and chronotropic effects can induce myocardial ischemia in case of significant stenosis of a coronary artery. Ischemia leads to hypo- or akinesia in the supplying territory of the artery. Echo has the ability tot detect these new wall motion disorders. Low dose DSE is also used to detect contractile reserve in damaged myocardium after infarction. The test performance for the detection of coronary stenosis is similar to myocardial perfusion imaging and superior to exercise ECG. Initially, images are made in rest: PLAX, PSAX pm, AP4Ch and AP2Ch. During dobutamine infusion, the patient should be monitored using a 12-channel ECG and blood pressure monitor. With each step of increasing dose of dobutamine (every three minutes, see table), an ECG and blood pressure measurement should be performed. A DSE test is safe, but can cause symptoms such as: palpitations, chest pain, dizziness or light-headedness. The dobutamine infusion should be terminated when the target heart rate [(220-age) x 0.85] is reached, serious complications or incidents occur, demonstrable new wall motion abnormalities in more than one segment are observed, or with an increase in end-systolic volume. In cases where the target heart rate has not yet been reached, one should consider to add atropine 0.25mg i.v., also be administered with a maximum of 1 mg (at intervals of 1 minute). At the target heart rate echocardiographic imaging using PLAX, PSax pm, AP4Ch and AP2Ch has to be performed exactly as the rest images to allow for proper comparison. This requires a strict routine of the sonographer. The last step is to ensure that the heart rhythm is back to normal.