Contrast agents
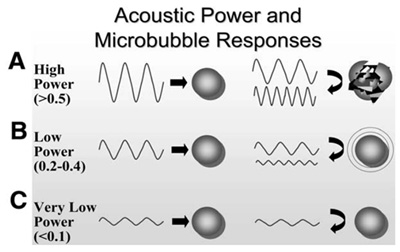
Commercially available contrast media are gas-filled microbubbles that are administered intravenously to the systemic circulation. Microbubbles have a high degree of echogenicity (the ability of an object to reflect ultrasound waves). ‘Left-sided’ contrast echocardiography uses these microbubbles to enhance the image quality of the left ventricular cavity. At the same time it can provide information about myocardial perfusion. Contrast echocardiography enhances the amplification of the echo signal of blood (better signal/noise ratio) and is used only in patients who have been unsuccessful without contrast (if there are two or more sections of LV myocardium are not able to judge). Contrast highlights the left ventricle cavity and strengthens the markings of the endocardial border, thereby improving accuracy in detection of regional wall motion abnormalities and assessment of intracavitary thrombus.