Quantification of tricuspid regurgitation
| Grading the severity of TR |
| TR severity classes |
Mild |
Moderate |
Severe |
| Qualitative parameters |
| Valve morphology |
Normal or mild abnormal leaflets |
Moderately abnormal leaflets |
Severe valve leasions/flail/large coaptation defect/ severe tenting |
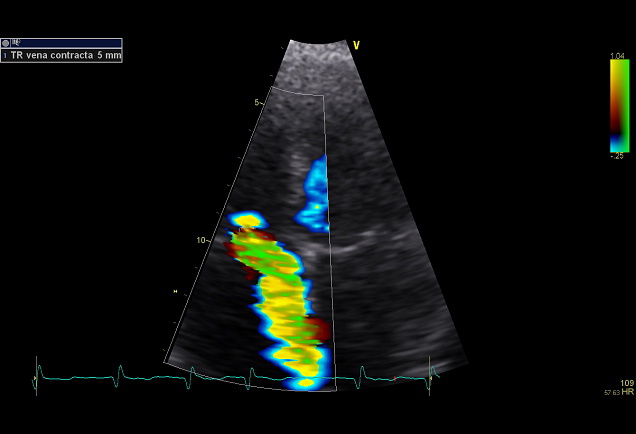
| Colour flow TR jet 𝛼 |
Small, narrow, central |
Moderate central |
Large central or eccentric wall impinging jet of variable size |
| Flow convergence zone |
Not visible, transient or small |
Intermediate in size and duration |
Large throughout systole |
| CW signal |
Faint/partial/parabolic |
Dense/parabolic or triangular |
Dense/often triangular with early peaking (peak <2m/s in massive TR) |
| Semi-quantitative parameters |
| Hepatic vein flow 𝛽 |
Systolic dominance |
Systolic blunting |
Systolic flow reversal |
| Tricuspid inflow |
A-wave dominant |
Variable |
E-wave dominant (≥ 1m/s) 𝜀 |
| PISA radius (mm) 𝛾 |
≤5 |
6-9 |
>9 |
| VC width (mm) 𝛼,𝛿 |
<3 |
3-6,9 |
>7 |
| 3D VC area or EROA (mm²) |
|
|
75-94 |
| Quantitative parameters |
| EROA (mm²) |
<20 |
20-39 |
≧40 |
| R Vol (mL) |
<30 |
30-44 |
≧45 |
| RF (%) |
≦15 |
16-49 |
≧50 |
| Structural parameters |
| RV, RA, IVC size 𝜁 |
Usually normal |
Normal or mild dilation |
Usually dilated |
CW, continuous wave; EROA, effective regurgitant orifice area; RA, right atrium; RV right ventricle; TR, tricuspid regurgitation; RF, regurgitant fraction; R Vol regurgitant volume; VC, vena contracta.
𝛼 At Nyquist limit of 50-60 cm/s.
𝛽 Unless other reasons, of systolic blunting (Atrial fibrillation, elevated RA pressure).
𝛾 Baseline Nyquist liit shift of 28cm/s.
𝛿 When VC width is assessed as an average ofmeasurements performed biplane the treshold value for severe TR is >9mm.
𝜀 In the absence of other causes of elevated LA pressure and of mitral stenosis.
𝜁 Unless for other reasons, the RA and RV size and VCI are usually normal in patients with mild TR, An end-systolic RV eccentricity index >2 is in favour of severe TR. In acute severe TR, the RV size is often normal. In chronic severe TR, the RV is classically dilated. Accepted cut-off values for non-significant right-sided chambers enlagement (measurements obtained from the apical four-chamber view): mid RV dimension ≤33mm, RV end-diastolic area ≤28cm², RV end-systolic area ≤16cm², RV fractional area change >32%, maximal 2D RA volume ≤33mL/m². An IVC diameter <21mm in considered normal. The IVC is dilated when the diameter is >25mm.
Echocardiographic criteria for the definition of severe tricuspid valve regurgitation: an integrative approuch.
| Parameter |
Criteria |
| Qualitative |
| Valve morphology |
Abnormal/flail/large coaptation defect |
| Colour flow regurgitant jet |
Very large central jet or eccentric wall impinging jet * |
| CW signal of regurgitant jet |
Dense/triangular with early peaking (peak <2 m/s in massive TR) |
| Semiquantitative |
| Vena contracta width (mm) |
≥ 7 * |
| Upstream vein flow |
Systolic hepatic vein flow reversal |
| Inflow |
E-wave dominant ≥ 1 m/s ** |
| PISA radius (mm) |
> 9 *** |
| Quantative |
| EROA (mm²) |
≥ 40 |
| Regugitant volume (mL/beat) |
≥ 45 |
| Enlargement of cardiac chamber/vessels |
RV, RA, IVC |
* At Nyquist limit of 50-60 cm/s.
** In the absence of other causes of elevated LA pressure
*** Baseline Nyquist limit shift of 28 cm/s.
| Outcome-based cut-off values for the quantitative parameters used to grade tricuspid regurgitation severity by Dopplerechocardiography. |
|
|
| Variable |
Low risk |
Intermediate risk |
High risk |
|
|
| VC (mm) |
<3 |
3 - 6 |
>6 |
|
|
| EROA (cm²) |
<0.15 |
0.15 - 0.30 |
>0.30 |
|
|
| RegVol (ml) |
<15 |
15 - 30 |
>30 |
|
|
| RegFR (%) |
<25 |
25 - 45 |
>45 |
|
|
| EROA, effective regurgitant orifice area; RegFr, regurgitant fraction; RegVol, regurgitant volume; VCavg, vena contracta width. |
|
|
| Eur Heart J Cardiovasc Imaging (2021) 22, 155-165 |
|
|
| |
| Proposed expansion of the ‘Severe’ grade |
|
|
|
|
|
| Variable |
Mild |
Moderate |
Severe |
Massive |
Torrential |
| VC (mm) |
<3 |
3 - 6.9 |
7 - 13 |
14 - 20 |
≥21 |
| EROA (cm²) |
<0.20 |
0.20 - 0.39 |
0.40 - 0.59 |
0.60 - 0.79 |
≥80 |
| 3D VCA or quantitative EROAa (cm²)* |
|
|
0.75 - 0.94 |
0.95 - 1.14 |
≥1.15 |
| VC, vena contracta; EROA, effective regurgitant orifice area; 3D VCA, three-dimensional vena contracta area. |
| *3D VCA and quantitative Doppler EROA cut-offs may be larger than PISA EROA. |
| Eur Heart J Cardiovasc Imaging (2017) 18, 1342–1343 |
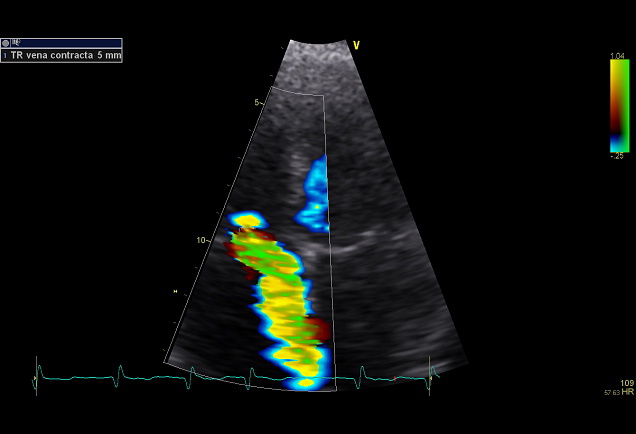
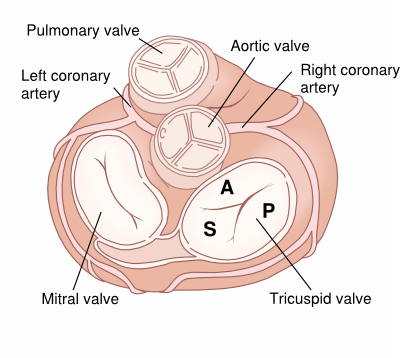
TR vena contracta
Causes of tricuspid regurgitation
| Functional TR |
Secundary TR |
| Disorders of the right ventricle: RV infarction, dilated cardiomyopathy |
Ebstein anomaly |
| Secondary to pulmonary hypertension, for example: cor pulmonale, pulmonary embolism, or primary. |
Infective Endocarditis |
| Mitral stenosis or mitral regurgitation |
Trauma |
| Left-right shunt, such as an atrial septal defect or a ventricular septal defect |
Rheumatic fever |
| Eisenmenger syndrome (rare) |
Carcinoid |
| Pulmonary stenosis |
Papillary muscle disorders |
| Hyperthyroidism |
Connective tissue diseases such as Marfan Syndrome. |
| |
Non-infectious endocarditis, such as SLE or rheumatoid arthritis |
| |
Damage from the electrode of a pacemaker or ICD |